Keeping Elevators Safe From Infections
Apr 1, 2021

Assessing the risks of picking up COVID-19 or other viruses or bacteria in a cab and how to reduce infection risk
by Dr. Michael Davies and Dr. P.J.B. Scott
There are many claims that elevators are a source of spreading coronavirus. However, there are only a small number of convincing cases where the use of elevators was involved in spreading the virus from one person to another. These instances are rare, because exposure times are short, and elevators are generally safe from infection transmission. It is, however, understandable that people are nervous about entering an enclosed space with strangers, and there are some simple, practical steps that can be taken to alleviate these concerns.
COVID-19 can be transmitted through direct contact of contaminated surfaces or from airborne droplets. Recent research has concluded that airborne droplets and tiny aerosols are the major source of transmission, but both can be significantly reduced by changes in behavior when using elevators.
Immediately available and relatively cost-effective solutions include:
- Keeping elevator doors open when idle and for longer when in use (where possible under local codes)
- Leaving ventilation systems on during idle operation
- Decreasing elevator capacity by encouraging stair use
- Reducing permitted elevator loading
- Distanced queuing and floor markings
- Staggered arrival, departure and lunchtimes
- Wearing masks and avoiding talking
- Using objects (pen, tissues, sanitary wipes, etc.) to avoid touching elevator buttons
- Provision and use of hand sanitizers
The addition of air circulation or purification systems, such as UV, ionizing treatments, installation of high-efficiency particulate air (HEPA) filters or changes in direction of airflow in the cabin have also been suggested as possible solutions. These all require expensive refits, can cause maintenance and ongoing cost issues and are probably unnecessary, especially if the measures listed above are adopted.
Retrofitting of contactless buttons can be done in a reasonable timeframe but is costly and may be unnecessary, since contact transmission is uncommon. Changing the materials of elevator walls, buttons and other surfaces is really only practical when designing new buildings and it is almost certainly an unnecessary expense.
How COVID-19 Is Transmitted
Respiratory viruses, including COVID-19, are transmitted in two main ways.[1-2] These need to be considered individually. The first is contact transmission, where someone comes into direct contact with an infected person or touches a surface that has been contaminated. The second is contactless transmission through the air. This method is divided into two types, depending on the size of contaminated droplets and how long they stay airborne:
Transmission of both large and small respiratory droplets that contain the virus, which would occur when near an infected person: facemasks and shields offer protection from larger droplets.
Airborne transmission of smaller droplets and particles (aerosols) suspended in the air over longer distances and times than droplet transmission. Respiratory aerosols are expelled from the infected person through breathing, coughing, sneezing, singing, talking, etc. and can reach the eyes, nose and mouth of any people nearby. Effectiveness of facemasks and shields against airborne transmission is less certain.
Contact Transmission
Contact transmission occurs if contaminated droplets land on surfaces that are then contacted by other people. Viable COVID-19 virus has been shown to remain viable on contaminated surfaces (fomites) for hours or even days. Remaining infectious time depends on temperature, humidity and the composition and nature of the surface.
The latest research suggests that direct contact with contaminated surfaces is unlikely to be a major route of transmission. Although SARS-CoV-2 can persist for days on inanimate surfaces, attempts to culture the virus from these surfaces have been unsuccessful.[3]
A review of literature on contact transmission showed that most studies have been done under experimental conditions.[4] For example, in the studies that used a sample of 107, 106, and 104 particles of infectious virus on a small surface area, these concentrations are a lot higher than those in droplets in real-life situations, with the amount of virus deposited on surfaces likely to be several orders of magnitude smaller. A representation of a real-life situation found no viable virus on fomites. The chance of transmission through inanimate surfaces is very small and only in instances where an infected person coughs or sneezes on the surface, then someone else touches that surface soon (1-2 h) after the cough or sneeze. Although periodically disinfecting surfaces and the use of gloves are reasonable precautions, especially in hospitals, fomites that have not been in contact with an infected carrier for many hours do not pose a measurable risk of transmission in non-hospital settings. A more balanced perspective is needed to curb excess cleaning/disinfecting that may be counterproductive.
The latest research suggests that direct contact with contaminated surfaces is unlikely to be a major route of transmission.
Non-Contact Transmission
Viruses in droplets (larger than 100 µm) can be sprayed like tiny cannonballs onto nearby individuals but typically fall to the ground in seconds within 2 m of the source. Because of their limited travel range, physical distancing reduces exposure to these droplets.[5] Aerosols (smaller than 100 µm) are generated during normal talking and breathing.
Large droplets were observed to fall onto the ground rapidly in a laser study.[6] Although the speed of the drops ranged 2–7 m/s at the start of a cough, the visible large drops (typically 500 μm in diameter) do not travel far before their trajectory bends down, due to gravity, to rapidly fall onto the ground within 1 s. From a sneeze, very large drops, originating from both the buccal and nasal cavities, were not persistent. Droplets coming from the nasal cavity with normal breathing were not detected above the background noise level.
Small droplets of a typical 5-μm radius have been calculated to take 9 min to reach the ground when produced at a height of 160 cm (i.e., average speaking or coughing height) in unventilated settings. Time to settling is heavily dependent on ventilation. In one study, in the best-ventilated room (with open door and window), the number of droplets had halved after 30 s. In a poorly ventilated room, the half-life was 1.4 min. With no ventilation, aerosols took about 5 min to settle.[6]
Initially, it was thought airborne aerosol transmission of COVID-19 was unlikely, but growing evidence has highlighted that infective microdroplets are small enough to remain suspended in the air and expose individuals at distances beyond 2 m from an infected person. Airborne transmission has been shown to occur during medical procedures that generate aerosols.[1] The World Health Organization (WHO) and scientists have been evaluating whether COVID-19 may also spread through aerosols in the absence of medical aerosol-generating procedures, particularly in indoor settings with poor ventilation. They concluded that aerosol transmission, combined with droplet transmission (for example, during choir practice, in restaurants or in fitness classes) is possible. In these events, short-range aerosol transmission, particularly in specific indoor locations, such as crowded and inadequately ventilated spaces over a prolonged period with infected persons, cannot be ruled out. This is also corroborated by investigation of the spread of cases between people not in direct or indirect contact, suggesting aerosol transmission was the most likely route.[1]
Viruses in aerosols can remain suspended in the air for many seconds to hours, like smoke, and be inhaled. They are highly concentrated near an infected person, so they can infect people most easily in proximity. But, aerosols containing infectious virus can also travel more than 2 m and accumulate in poorly ventilated indoor air, leading to superspreading events.[7] Cases of transmission from people more than 2 m apart have occurred, but this has been in enclosed spaces with poor ventilation and typically with extended (more than 30 min of) exposure to an infected person.[2] In an analysis of 75,465 COVID-19 cases in China, 78-85% of clusters occurred within household settings, suggesting transmission occurs during close and prolonged contact.[8] Outside of the household setting, those who had close physical contact, shared meals or were in enclosed spaces for approximately 1 h or more with symptomatic cases, such as in places of worship, gyms or the workplace, were also at increased risk of infection.[1]
In summary, the transmission of COVID-19 is likely by close contact for prolonged periods (30 min or more) with someone with symptomatic infection. It is less clear whether asymptomatic people can infect others, but it has been found that pre-symptomatic people can transmit before their symptoms develop. It is also likely that aerosol transmission is occurring, particularly in poorly ventilated indoor spaces.
COVID-19 Transmission in Elevators
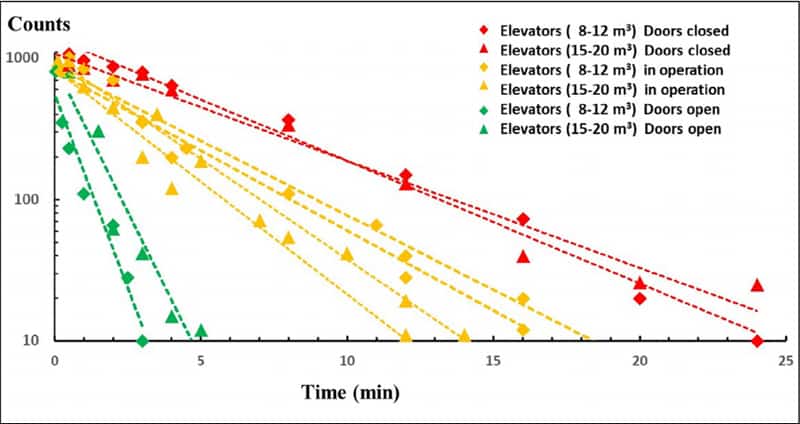
An important experiment was conducted inside elevator cabins in a hospital during normal operation with about 10-20% open door time.[9] Typically, it took 12-18 min before the number of aerosol particles decreased 100fold during normal operation of both medium-sized and large cabs. With elevator doors permanently open, this time was reduced to 2-4 min (Figure 1). In all cases, the number of aerosols decreased exponentially over time. There have been few well-documented cases of COVID-19 transmission in elevators.
Case 1: Outbreak in Office Building Call Center in South Korea
An outbreak occurred in March 2020 in building X, a 19-story building in one of the busiest urban areas of Seoul. Commercial offices are on floors 1-11, and residential apartments are on floors 13-19. 922 employees who worked in the commercial offices, 203 residents who lived in the residential apartments and 20 visitors were identified and investigated. The call center is on floors 7-9 and 11; it has a total of 811 employees. Employees do not generally go between floors, and they do not have an in-house restaurant for meals.
The first case patient, who worked in an office on the 10th floor (and reportedly never went to the 11th floor), had an onset of symptoms on February 22. The second case patient, who worked at the call center on the 11th floor, had an onset of symptoms on February 25. Residents and employees in building X had frequent contact in the lobby or elevators. It was not possible to trace back the index case patient to another cluster or an imported case. There were 97 confirmed COVID-19 patients in building X, indicating an attack rate of 8.5%. The attack rate was as high as 43.5% when restricting the results to the 11th floor.
Nearly all the case-patients were on one side of the building on the 11th floor. Despite considerable interaction between workers on different floors of building X in the elevators and lobby, COVID-19 spread was limited almost exclusively to the 11th floor, which indicates that the duration of interaction (or contact) was likely the main facilitator for its further spread.
There have been few well-documented cases of COVID-19 transmission in elevators.
Case 2: Transmission in an Apartment Building in China
Transmission of COVID-19 through contact with elevator surfaces was found in China.[11] One patient, B1.1, was the downstairs neighbor of the first patient, A0. They used the same elevator in the building, but not at the same time, and did not have close contact otherwise. Patient B 1.1 went on to infect family and friends, who infected more family and friends, resulting in an outbreak of 71 cases. This case is sometimes cited under the headline, “Woman infected 71 people with COVID-19 through single elevator trip in China, report finds.”[12] However, only one case of transmission through contact with elevator surfaces was found. This case was also quoted by a company selling air-filtration systems for elevators as, “6/30/20 CDC release, contact trace report: one woman infects over 70 people in one 60-s elevator ride.” These clearly inflammatory headlines and quotes do not reflect an accurate picture of the situation.
Reducing the Risk of Transmission in Elevators
If people follow the current guidelines about the virus, i.e., wearing effective face coverings, properly practicing hand hygiene and keeping socially distanced, the danger of transmitting the virus in elevators is small. There are, however, some things that can be done to further reduce the risk of transmission. Some require some simple behavioral changes, while others require engineering or control modifications.
Behavior
There are several published guides intended to decrease the likelihood of transmission of COVID-19 in elevators.[9 & 13-15] Their recommendations can be summarized into categories of those measures under the control of building managers or tenants and those of individual elevator etiquette. A list of the former is:
- Leave elevator doors open for longer and when the elevator is idle. This will depend on local codes and may not be possible at the lobby level. HVAC balance will also need to be considered.
- Encourage stair use, particularly for interfloor traffic, with fixed directions up and down, one way, where possible.
- Consider a physical operator/designated attendee engaged to enter hall calls or destination-dispatch requests.
- Organize queuing, more so in the first few days of each phase involving relaxation of restrictions.
- Reduce capacity for elevators, such as four for larger cabs and two for smaller ones.
- Building tenants could adopt a shift in schedules (start early or late, and leave early or late). This requires calculations of handling capacity.[16]
- Encourage lunch at desks over a staggered timeframe (three lunch hours at 11 a.m.-2 p.m. is better than noon-1 p.m. for everyone; 12:45 p.m. is generally the busiest time for office elevators).
- Promote food service providers in/near the building offering a delivery service.
- Use floor markings in elevator lobbies and near the entrance to escalators to reinforce social distancing. Place decals inside the elevator to identify where passengers should stand, if needed.
- Use stanchions (for lobbies only; not inside elevators) or other ways to mark pathways to help people travel in one direction and stay 6 ft apart.
- Consider limiting the number of people in an elevator and, where possible, leaving steps empty between passengers on escalators.
- Supply hand sanitizers, where possible.
- Post signs reminding occupants to minimize surface touching.
- Consider adding supplemental air ventilation or local air-treatment devices in frequently used elevator cars.
- Enhance cleaning of elevators (for example, hourly), depending on usage and on any local public health direction.
- Consider those with disabilities: those in wheelchairs may not be able to travel into or out of one quadrant of an elevator; those with vision challenges may need assistance in where to stand in an elevator.
Individual behavior in an elevator can go a long way to ameliorate the risk of contamination. These recommendations should be posted and/or circulated to building inhabitants. Surgical masks can contain, and therefore reduce, the dissemination of viruses shed by an infected wearer by up to fourfold (75%) and even 100% in the case of seasonal coronaviruses. When an infectious person wears a mask or face covering, the size of the exhaled plume is also reduced. This also helps reduce the risk of exposure to those nearby. Surgical masks also protect the wearer by reducing the exposure to incoming droplets and aerosols from infected individuals by an average of sixfold (range: 1.1fold to 55fold).[17] Elevator users should follow the following etiquette rules:
Wear cloth face coverings.
Stand on the markers, where provided, facing the direction indicated.
Announce your floor to the person closest to the buttons.
Avoid speaking when possible.
If you must cough or sneeze, turn to the wall and cough into your elbow with your mask on.
Avoid touching your face after holding handrails or touching buttons, and use any available hand sanitizers.
Use an object (such as a pen, tissue or sanitary wipe) or knuckle to push elevator buttons.
If the elevator is busy, wait for the next one.
When the door opens at a floor, people in the middle should move to the side, and people in the front should move outward to create exit pathways.
Additional air circulation might disperse aerosols, but this is unlikely to reduce transmission if air is recirculated without filtration or treatment.
Ventilation
The atmosphere in a lift manufactured in complete accordance with EN 81-1, installed in a fully air-conditioned building, with the car fan switched off, became life-threatening when occupied with a full load of passengers after only 30 min.[18] (Note that EN 81-1 has been replaced by EN 81-20/-50.) Building to ASME A17.1/CSA B44 provides more ventilation, and many elevator cabins are built to other national standards. Many lifts are installed in buildings without air-conditioning and located in tropical and subtropical regions, where air temperatures exceed 46˚C, and humidity exceeds 50% (apparent temperature: 66˚C). Even a single person trapped for only a short time is at great risk. The cabin ventilation requirements in the current codes might need to be revised.
Researchers of aerosol transmission in hospital elevators recommend elevator doors be left open for a longer period whenever possible.[9] It was found that the ventilation inside all studied elevators in an idle position automatically shut off after 1-2 min. The authors suggested that door opening should be prolonged by reprogramming the action control software to reduce contamination. Another suggestion was to reverse the flow direction of the ventilator, creating a unidirectional downflow of fresh (e.g., HEPA-filtered) air from the ceiling toward the floor of the cab.
Air-circulation fans have been suggested as possibly being helpful. KJA Consultants Inc. has looked at this possibility and notes that, currently, most fans do not have filters. The company says it has experienced nonfunctional fans. Additional air circulation might disperse aerosols, but this is unlikely to reduce transmission if air is recirculated without filtration or treatment. A study of influenza infection risk in cars with low, medium and high ventilation of circulating air suggested that infection risk can be reduced by not recirculating air. Estimated risk ranged from 59% to 99.9% for a 90-min trip when air was recirculated.[19] It has not been demonstrated that merely circulating the air will reduce transmission, compared with introducing more fresh air and removing stale air more effectively.
Copper-containing surfaces will reduce the lifetime of droplets landing on them after several hours or days, but copper materials are unlikely to be a viable solution, because elevator surfaces may be touched every few seconds or minutes.
Fans with filters are an improvement over air-recirculating fans. They would, however, require additional maintenance (replacing filters, for example) and increase the weight that might trigger rebalancing and other work. Adding components would also make it less safe for the mechanic to work on top of the car. The best practice would probably be to have HEPA-filtered downflow fresh air constantly during operation, doors open and fans on for at least 4 min, where possible, but note comments about maintenance.
UV and air ionizing treatments are being offered commercially but would suffer from the same problems as air-circulation fans. There also seems to be little direct evidence this would substantially reduce transmission in elevators.
Materials
KJA has reviewed how surfaces of different materials become contaminated.[20] Microbes can live for varying lengths of time, from up to five days on glass to several hours on cardboard and pure copper. Copper-containing materials are known to deactivate microorganisms, and this type of material is being offered for cab interiors. Copper-containing surfaces will reduce the lifetime of droplets landing on them after several hours or days, but copper materials are unlikely to be a viable solution, because elevator surfaces may be touched every few seconds or minutes.[21] It is known that sweat can corrode copper alloys, like brass, in the long term. Researchers recently found that, within as little as 1 h, the salt in sweat can form a corrosive layer on the surface of the metal, which would prevent the electrochemical reaction that kills microorganisms.[22] Some cleaning solutions may also coat the copper surface and inhibit its biocidal activity.[21]
Passenger behavior, particularly the proper wearing of masks and not speaking, can significantly reduce the risk of transmission in cabs.
Touchless Controls
There are many commercial products that can convert elevators into touchless operation to reduce the small risk of transmission by contact. These include glass-fronted touchscreens sealed like a smartphone so they can withstand disinfection, and touchless call buttons that will summon an elevator with the wave of a hand or direct it with a hovering finger.[23] Another technology uses a hologram to project virtual buttons into the air.
Advanced destination-dispatch systems are tied into turnstiles, where employees swipe their cards for entry to office towers. The system automatically summons an elevator and directs the user to which one to take. Other systems use an app tied into proximity sensors, but connectivity remains a challenge.
Finally, large floor-mounted buttons in halls and elevators can be hit with a shoe, avoiding the need to touch buttons with a finger.
References
[1] WHO. “Transmission of SARS-CoV-2: implications for infection prevention precautions”, (WHO/2019-nCoV/Sci_Brief/Transmission_modes/2020.3), p. 10 (2020).
[2] The Lancet. “COVID-19 transmission — up in the air” (www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30514-2/fulltext) (2020).
[3] Mondelli, et al. “Low risk of SARS-CoV-2 transmission by fomites in real-life conditions,” The Lancet Infectious Diseases (doi.org/10.1016/ S1473-3099(20)30678-2) (September 29, 2020).
[4] E. Goldman, “2020 Exaggerated risk of transmission of COVID-19 by fomites,” The Lancet. (doi.org/10.1016/ S1473-3099(20)30561-2) (July 3, 2020).
[5] Prather, et al. “Airborne transmission of SARS-CoV-2” (science.sciencemag.org/content/370/6514/303.2/tab-pdf).
[6] G. Aernout Somsen, et al. “Small droplet aerosols in poorly ventilated spaces and SARS-CoV-2 transmission,” The Lancet. (doi.org/10.1016/S2213-2600(20)30245-9) (May 27, 2020).
[7] S. L. Miller, et al. Indoor Air, (doi.org/10.1111/ina.12751) (2020).[5]
[8] WHO. “Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 16-24 February 2020,” Geneva, Switzerland (www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf) (2020).
[9] C. van Rijn, et al. “Reducing aerosol transmission of SARS-CoV-2 in hospital elevators,” Indoor Air, Vol. 30(6) (onlinelibrary.wiley.com/doi/10.1111/ina.12744).
[10] Park, et al. “2020 Coronavirus Disease Outbreak in Call Center, South Korea.” Emerging Infectious Diseases, Vol. 26, No. 8 (www.cdc.gov/eid) (August 2020).
[11] J.T. Liu. “Large SARS-CoV-2 Outbreak Caused by Asymptomatic Traveler, China,” Emerging Infectious Diseases, Vol. 26, No. 9, September 2020: 2260-2263 (www.cdc.gov/eid).
[12] H Brewis. Woman infected 71 people with COVID-19 through single elevator trip in China, report finds, Evening Standard News (July 13, 2020).
[13] KJA. “COVID-19 PANDEMIC 2020, Post Pandemic Action Plan – VT Considerations,” (www.kja.com/2020/05/06/kja-covid19-post-pandemic-considerations).
[14] BOMA Canada Coronavirus Working Group, “Pathway Back to Work” BOMA Canada, version 2, p. 9-10 (June 18, 2020).
[15] CDC, “COVID-19 Employer Information for Office Buildings” (January 2021).
[16] KJA. “How to manage Elevator Service in buildings under Social Distancing Restrictions” (www.kja.com/2020/05/05/how-to-manage-elevator-service-in-buildings-under-social-distancing-restrictions).
[17] J.W. Tang, W.P. Bahnfleth, P.M. Bluyssen, G. Buonanno, J.L. Jimenez, J. Kurnitski, Y. Li, S. Miller, C. Sekhar, L. Morawska, L.C. Marr, A.K. Melikov, W.W. Nazaroff, P.B. Nielsen, R. Tellier, P. Wargocki and S.J. Dancer. “Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus (SARS-CoV-2), Journal of Hospital Infection, (doi.org/10.1016/j.jhin.2020.12.022).
[18] Rory S. Smith, “Cabin Ventilation, Code Requirements and Experimental Results”, 3rd Symposium on Lift & Escalator Technology (CIBSE Lifts Group, The University of Northampton and LEIA (2013; web version © Peters Research Ltd. 2019).
[19] L.D. Knibbs, L. Morawska and S.C. Bell. “The risk of airborne influenza transmission in passenger cars.” Epidemiology and Infection 2012; 140: 474–478.
[20] P.J.B. Scott and M. Davies, 2020 Contamination of surfaces in elevators and on escalators (www.kja.com/2020/05/05/contamination-of-surfaces-in-elevators-and-escalators).
[21] M. Davies and P.J.B. Scott. “Elevator Buttons – Antimicrobial properties of copper and copper alloys,” December 2020 (www.kja.com/2020/12/21/antimicrobial-properties-of-copper-and-copper-alloys).
[22] Bob Hirshon. “Antibacterial door knobs,” American Association for the Advancement of Science NetLinks.
[23] Meredith MacLeod, “New Normal: Elevators moving touchless, mobile and sideways,” CTV News (July 31, 2020).

Dr. P.J.B. Scott trained in biology and oceanography in Canada. Scott has, for many years, studied the effects of organisms, particularly microorganisms, on structures in underwater and wet environments and has extensive industrial experience in identification and remediation techniques of microbial attack on materials.
Get more of Elevator World. Sign up for our free e-newsletter.