Highlights of an airflow study conducted to determine the relative risk of exposure to COVID-19 among elevator passengers
by Stephen R. Nichols, Dr. Sumei Liu, Dr. Xingwang Zhao, Dr. James T. Auxier, Tricia Derwinski, Dr. Murilo Bonilha and Dr. Qingyan (Yan) Chen
Elevators play an essential role in keeping people around the world on the move every day. However, the global COVID-19 pandemic has created some concerns around the relative risk of infection in shared common spaces, including elevators. Early in the pandemic, stories began appearing in both popular and scientific publications raising questions about riding in elevators based on the understanding of airborne transmission as a critical means of disease spread and, at least in part, the misperception that elevator cabs are sealed spaces with limited airflow.
Study Overview
An understanding of elevator systems, ventilation and design, along with the nature of COVID-19, suggests that the relative exposure risk in elevators is lower compared with that of many other common spaces. However, it does not take into account the dynamics of specific situations, including passenger flow, ventilation rates, cab sizes and mitigation strategies that include masks and air purification.
To understand the true impact of these dynamics, Otis commissioned a team at Purdue University to conduct a study focused on understanding the relative exposure to COVID-19 in elevators. The study focused on airflow and investigated the impact of ventilation rates and types, purification technologies and interventions, including masks in elevator environments.
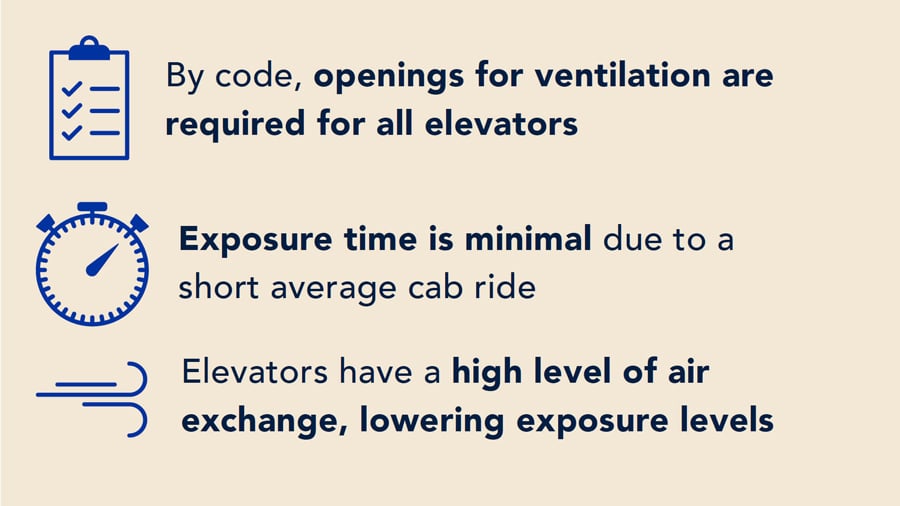
Elevators are, in fact, well-ventilated spaces. By code, elevators are required to have openings for ventilation. Together with fans commonly present in elevators, these openings provide a high level of air exchange. Exposure time to the air and other people in an elevator is also limited due to the short duration of the elevator ride — less than 2 min, on average, for the tallest buildings and on the order of 30 s for many rides. While this knowledge and a simple analysis suggest airborne transmission of aerosols and particles in elevators is much lower compared with that in many other common spaces, it does not take into account the dynamics of specific situations, including passenger flow, ventilation rates, cab sizes and mitigation strategies, including masks and air purification.
Every elevator riding scenario is different, with multiple variables important to the movement of people, air and elevators. Otis commissioned an elevator airflow research study to understand the impact of these dynamics and support our customers and the riding public with science-based information and solutions. The study focused on understanding the relative risk of COVID-19 exposure in elevators. We set out to learn how mitigation strategies and other factors impact using elevators during the pandemic. More specifically, the research team undertook the study to:
- Evaluate transmission risk of airborne particles infected with SARS-CoV-2 (the virus that causes the disease COVID-19) when taking an elevator
- Study different elevator design parameters — including fan speed — that could have a major impact on the exposure risk
- Identify the impact of mitigation strategies and methods
- Compare the exposure risk of an elevator with that of other enclosed spaces, such as an office or a city bus
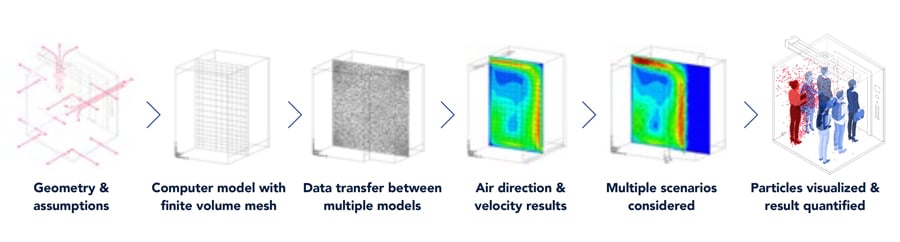
The investigation used multizone modeling to simulate airflow between zones across the envelope of a building and computational fluid dynamics to simulate particle dispersion during a 2-min elevator ride compared with time spent
in other common spaces. For the elevator ride, we modeled multiple scenarios, including particle dispersion when the doors open as passengers get on and off the elevator.
Coupled with what we already know about elevator design and operation, the findings of the study show that riding in an elevator is a relatively low-risk activity. The research has shown that the higher the level of air exchange, such as that provided by higher-flow elevator fans, the lower the exposure risk. When considering relative risks between common indoor activities, the study found that the elevator ride is comparable to a short time in an office or bus. However, when you consider the longer average duration of a stay in a bus or office compared to an elevator ride, we observed significantly less relative exposure risk in an elevator.
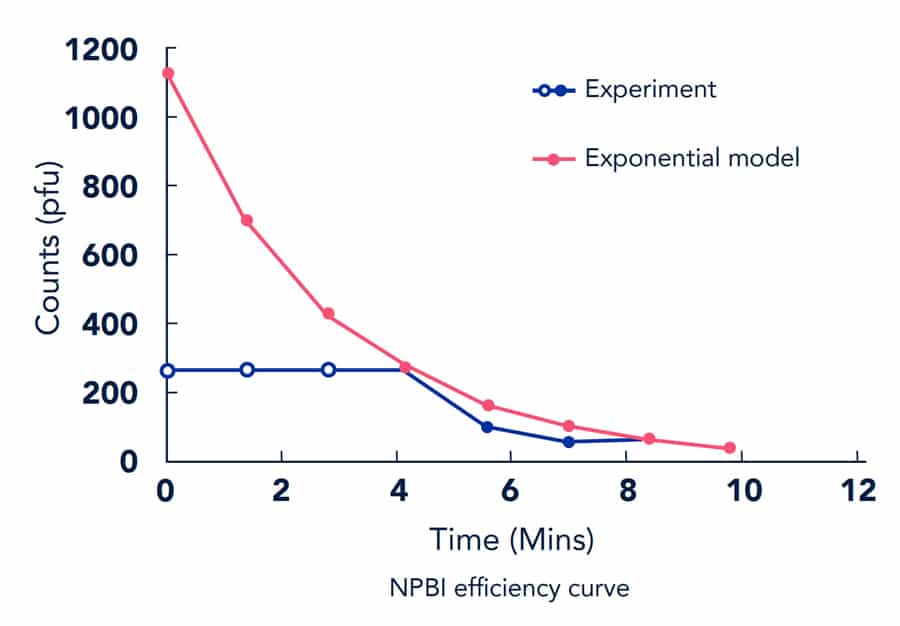
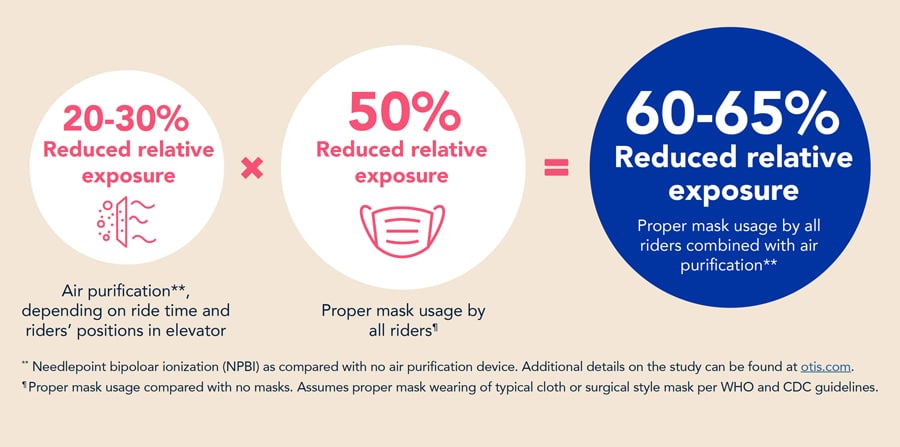
In addition, mitigation strategies were shown to reduce the risk even further. Proper mask usage cut the potential risk in half, air purification via needlepoint bipolar ionization (NPBI) reduced risk 20-30%, and combining the two strategies resulted in a 60-65% reduction in relative exposure. (For comparison details and more information, see graphic on p. ) While the calculations themselves don’t vary, the results of the calculations do vary, depending on ride time and riders’ positions in the elevator.
Assessing Risk and the Novel Coronavirus
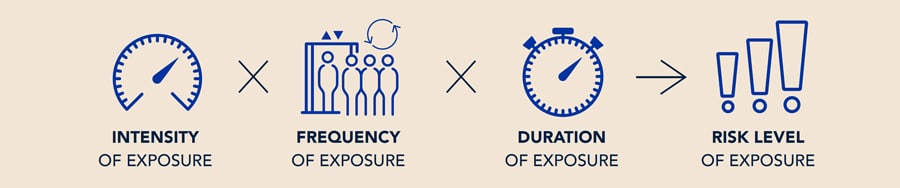
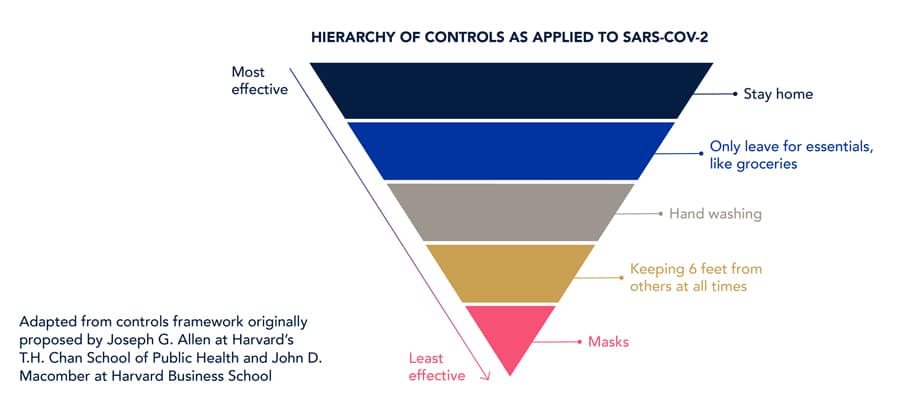
As the world continues to navigate the pandemic, and societies look for ways to resume aspects of everyday life, experts across disciplines recognize there is no “silver bullet.” A risk-based approach, informed by science, is needed to recommend reasonable control measures for each situation (Defile, 2020). Risk level is based on the intensity, frequency and duration of exposure. For each application, the level of exposure via airborne means or physical contact may be different. Not all applications can be easily compared without using a combination of techniques and different disciplines.
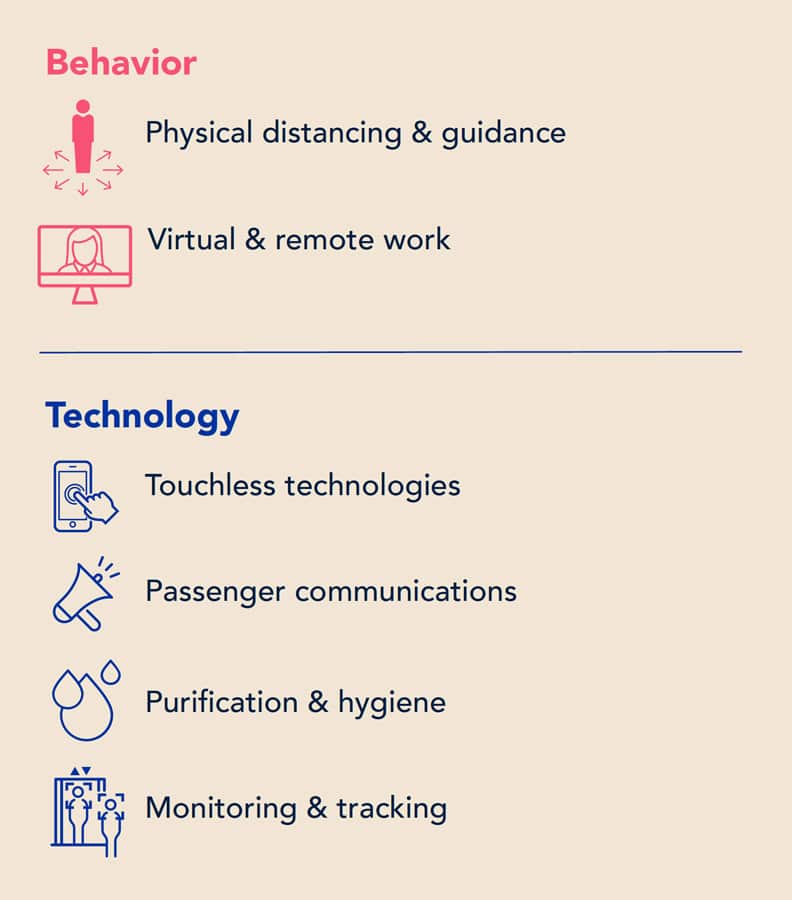
Through a risk-based approach, we are able to determine and prioritize elements of a layered strategy that encompasses both behavioral and technology recommendations, each with varying levels of effectiveness and disruption.
These broad principles are applicable in the case of elevators. As we look to address concerns around the relative risk of exposure in an elevator, several factors and scenarios need to be balanced to achieve a range of positive outcomes and solutions for Otis customers and the riding public. We need to account for the dynamics of not just the elevator, but also of the building environment and people’s behavior. Understanding relative risk and how to integrate different layers of control methods and solutions are key.
When considering responses to the current pandemic, these solutions primarily focus around four key areas:
- People and elevator movement
- Guidance for safe riding
- Exposure risk mitigation
- Advanced technology solutions
Additional considerations are driven by the vertical movement of the elevator, the opening and closing of doors, and the movement of people in and out of elevators, all within a reasonably small enclosure volume. Further, these factors must be viewed in the context of what science tells us about how COVID-19 travels through the air.
Examining COVID-19 Transmission
The World Health Organization (WHO), Centers for Disease Control and Prevention (CDC) and other experts indicate multiple modes of transmission for SARSCoV-2.
Emerging science and evidence seem to support that airborne transmission may be more critical than surface-to-surface transmission (WHO and Mandavilli, 2020). With the increasing emphasis on airborne transmission, the emphasis on indoor air quality and airflow continues to grow.
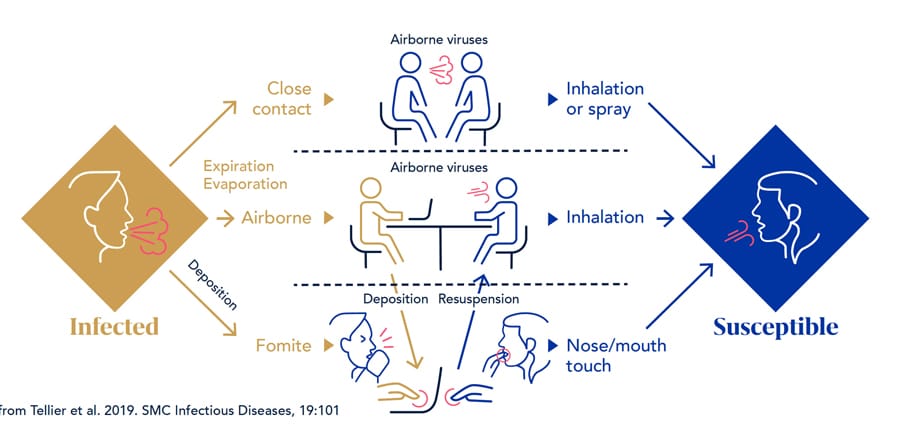
Airborne transmission either via large droplets or small aerosols depends on the particle size and amount inhaled. Different quantities of particles are exhaled during different situations. Breathing spreads fewer and smaller particles than coughing. The amount of time spent breathing, coughing or speaking is important, as is the distance and duration spent in close proximity to an individual and the airflow of how the particles move in space. The intensity of the exhalation, duration you are in proximity to an infected individual and frequency of contact may all contribute to the relative risk of infection spreading. A recent study shows virus concentration is different in various-sized particles. For example, virus concentrations are typically higher in the finer particles generated deep within the lungs and throat, which can be expelled through coughing. Conversely, particles generated from speaking mainly consist of saliva, which can contain lower virus content.
It is not just the number of particles in the air, but the impact of where these particles go and whether they are inhaled and rest either in the upper or lower parts of your lungs. We can model the particles and air, but we also need to take into account the relative accumulated dose of the particles for an individual in different scenarios. It is not necessarily sufficient to study airflow alone; understanding the concentration and distribution of the potentially infected particles dynamically at different times in different situations gives us a more accurate assessment of risk.
Many quick analyses may look at perfectly mixed air and simplify the situation. However, analyzing the movement of the air, people and elevator together provides more detail. For a complete analysis, further work could include detailed study of surface-to-surface or fomite (landed viral particles) transmission.
There are multiple ways to analyze airborne transmission and the spread of the virus using techniques from such fields as public health and medicine, engineering, mathematics and statistics, and network theory.
Understanding Elevators
In examining the relative risk of COVID-19 exposure in elevators, the science around airborne transmission of particles points us to focus on airflow. Though relatively small, modern elevator cabs are well-ventilated spaces with systems for circulating the air frequently.
Elevators have required ventilation standards. By code, openings are required for natural convection, and the majority of elevators have fans or can easily be retrofitted to have fans. Elevator fans are often sized to provide one air change per minute. Air changes per hour (ACH) are a measure of the air volume added to or removed from a space in 1 h, divided by the volume of the space. Higher values correspond to better ventilation.
By North American elevator code, cabs must provide 3.5% of the platform area as ventilation openings for convection purposes (American Society of Mechanical Engineers, 2019). European code EN 81-1, which is applied in much of the world, requires 2% ventilation, which is still a significant amount of openings, regardless of cab configuration (British Standards Institution, 2014).
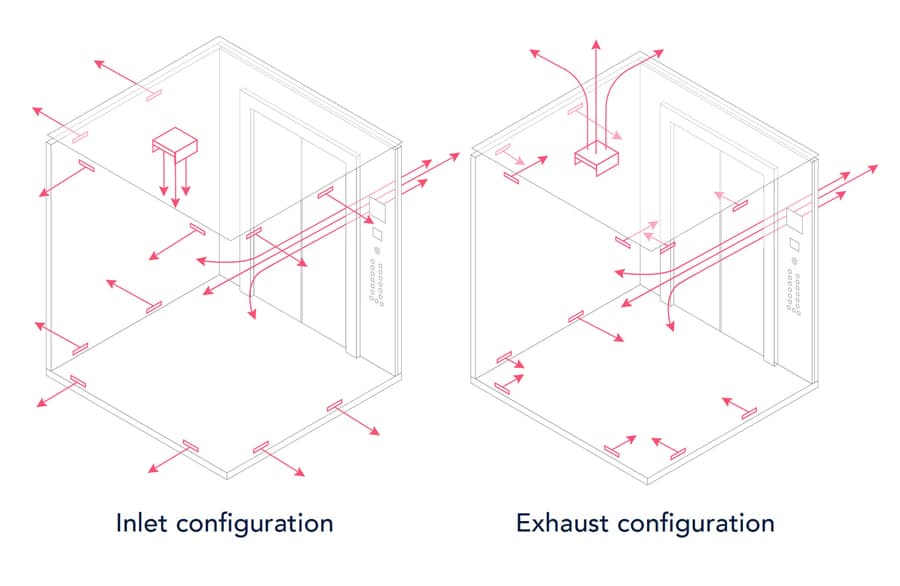
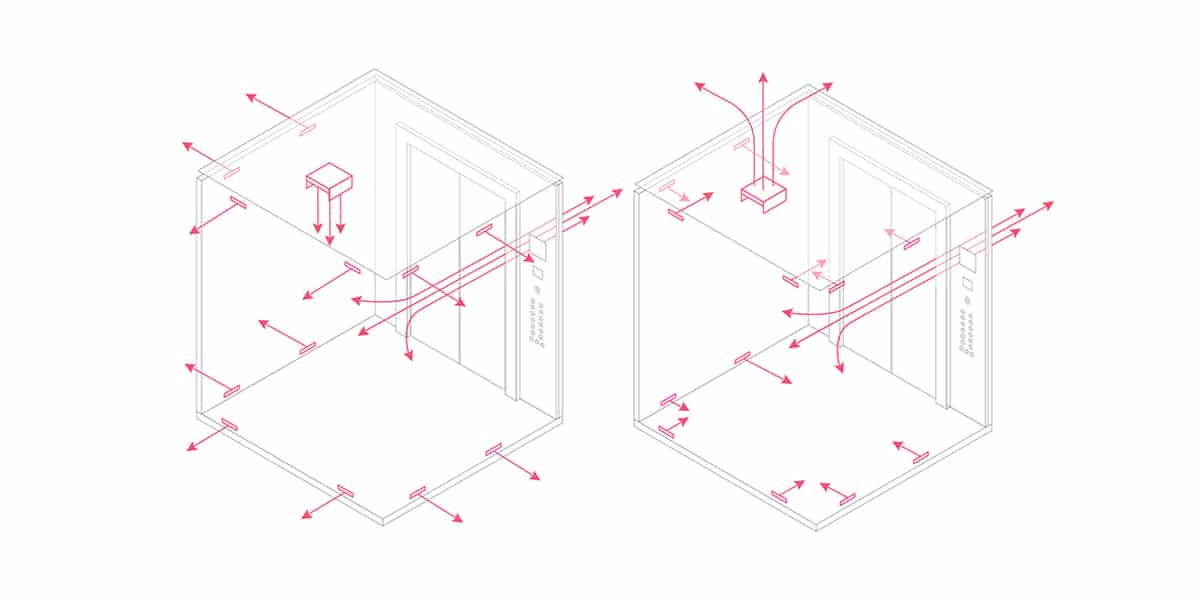
A System Within a System
When considering an elevator ride, we consider the air and space the passenger encounters in the cab itself, the hoistway or shaft and the other parts of the building where people are moving. The opening for the fan and the opening around the doors may be included in the calculation. These openings provide inlets and outlets for convective transfer of passive airflow and aid when more active ventilation is present. Depending on the complexity of the building, additional factors, including pressurization; fire considerations; and more sophisticated heating, ventilation and air-conditioning (HVAC) systems; and air movement between the elevator and the lobby or floors at different stops should also be considered.
Introduction to Airflow Modeling
Airflow is complex. It can be modeled in a computer and by measuring actual airflow in an experiment. Computer modeling is often recommended to study multiple scenarios and variables quickly. The computer modeling and numerical simulation methods used in this study are at the cutting edge in the state of the science.
For a single enclosed space, computational fluid dynamics (CFD) is the most powerful airflow and contaminant modeling tool. CFD has been widely used because it can provide informative and accurate results of transient particle transport in enclosed environments. There are two parts of CFD modeling on contaminant transport: airflow modeling and particle/particle modeling.
To obtain information about airflow distribution, CFD numerically solves a set of partial differential equations for the conservation of mass, momentum (Navier-Stokes equations), energy and turbulence quantities. The solution includes the distributions of air velocity, pressure, temperature, turbulence parameters and contaminant concentration.
To best simulate the elevator environment, we used a multizone model, as it is applied to multiple rooms connected with openings such as doors, windows and cracks. The multizone models also assume each zone to be a well-mixed space. Although the assumption that uniform air contaminant concentration in a zone may not be valid, it is sufficient for simulating airflow through cracks between an elevator cab and a hoistway and between a hoistway and lobbies. This is because the uncertainties in those large spaces are very high. The airflow through the small openings is more important than the uniformity of virus concentration distribution.
Reynolds-averaged Navier-Stokes (RANS) models are the most popular CFD models. RANS models solve the mean air variables, such as air velocity and temperature, and model turbulence properties by solving turbulence transport equations. For indoor airflow modeling, Zhang et al (2007) recommended the RNG k-![]() model after reviewing and comparing many models. This model was selected for the present study.
model after reviewing and comparing many models. This model was selected for the present study.
Although this research did not include experimental measurements, the numerical simulation technique was based on validated tools. For example, we used the Lagrangian model in CFD to simulate particle dispersion in a clean room (Murakami et al, 1992). We also compared the simulated and measured particle concentration distributions. The results of Lagrangian calculation were based on a sample size (i.e., the number of trajectories) of 100,000. The results are in reasonable agreement with the experimental data.
The Lagrangian particle tracking method could introduce uncertainty into particle concentration calculations. When the particle number is low, the predicted particle concentration may not be a stable solution due to the random factors used in the model. This can be seen in the results obtained in this project.
Study Modeling Methodology
Using the multizone computer modeling and numerical simulation methods outlined above, the study set out to examine potential exposure risk by simulating various elevator ride experiences.
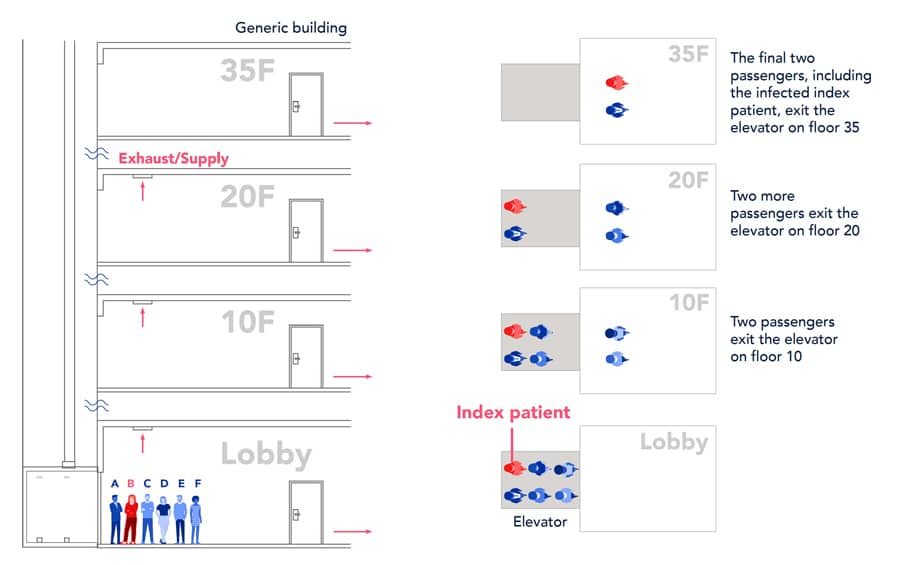
To consider the whole process when taking an elevator, we assumed an elevator ride scenario in a commercial building with 35 floors. Among the six riders, two riders left the elevator on floor 10, another two left on floor 20, and the other two left on floor 35. One of the two to floor 35 was an index patient, shown by the red color in the following figure. The longest trip took approximately 2 min.
This typical building and representative elevator journey allowed us to isolate variables and determine that the exact details of elevator speed or path were not as important as total time in each space.
This investigation used the multizone model, ContamW, to simulate airflow through cracks between an elevator cab and hoistway and between hoistway and lobbies. Results of the multizone airflow modeling were used as a part of the thermo-fluid boundary conditions for detailed simulations of COVID-19 virus particle transmission for the elevator ride. The detailed simulations used the previously described CFD technique with the Lagrangian method for particle dispersion. The simulations of the 2-min elevator ride were further divided into eight sub-cases for considering the changes of flow domains in the elevator ride. The particle and airflow distributions of the previous sub-case were used as initial conditions of the current sub-case to ensure smooth transfer of the data for accurate simulations of particle transmission in the elevator ride. The CFD used was Reynolds-averaged Navier-Stokes equations with the RNG k-![]() turbulence model built in the ANSYS Fluent computer program. ANSYS Fluent is one of the more sophisticated CFD codes available and is commonly used for advanced computer simulation.
turbulence model built in the ANSYS Fluent computer program. ANSYS Fluent is one of the more sophisticated CFD codes available and is commonly used for advanced computer simulation.
[A] typical building and representative elevator journey allowed us to isolate variables and determine that the exact details of elevator speed or path were not as important as total time in each space.
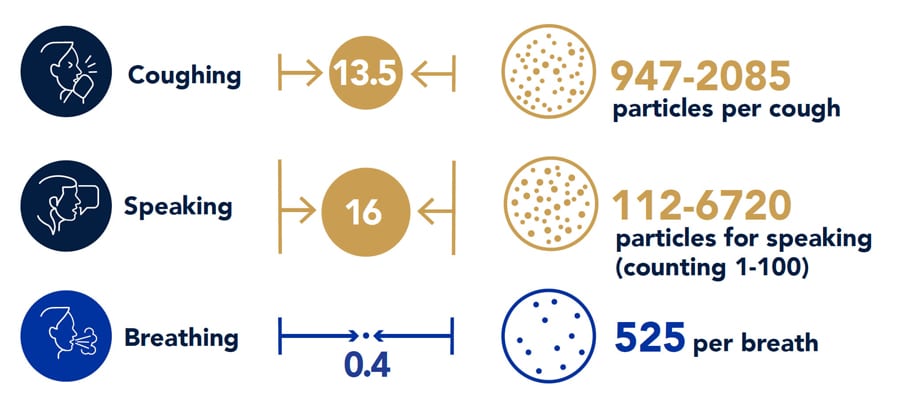
This investigation mainly considered the transmissions of airborne particles generated by breathing of the index patient. Each breathing cycle lasted 4 s and generated 525 particles with an average diameter of 0.4 µm. The research also studied a coughing case when the index patient coughed once when entering the elevator. The impact of different elevator design parameters on the particle transmission was also studied:
- Ventilation rate of 350 ft3/min, 150 ft3/min and 55 ft3/min and infiltration rate of 36 ft3/min
- Air blowing in and air blowing out
- Wide elevator cab and deep elevator cab
Since the study used particle number or particle mass inhaled by susceptible riders as the evaluation criterion, it could not show the absolute risk. Thus, we compared the exposure level to the particles in the elevator ride with that in an office and a bus.
This study investigated particle sources generated by an index patient through breathing and coughing. For breathing, the numerical simulation used an average particle size of 0.4 μm in diameter, with 525 particles per breathing cycle. Each breathing cycle lasted 4 s.
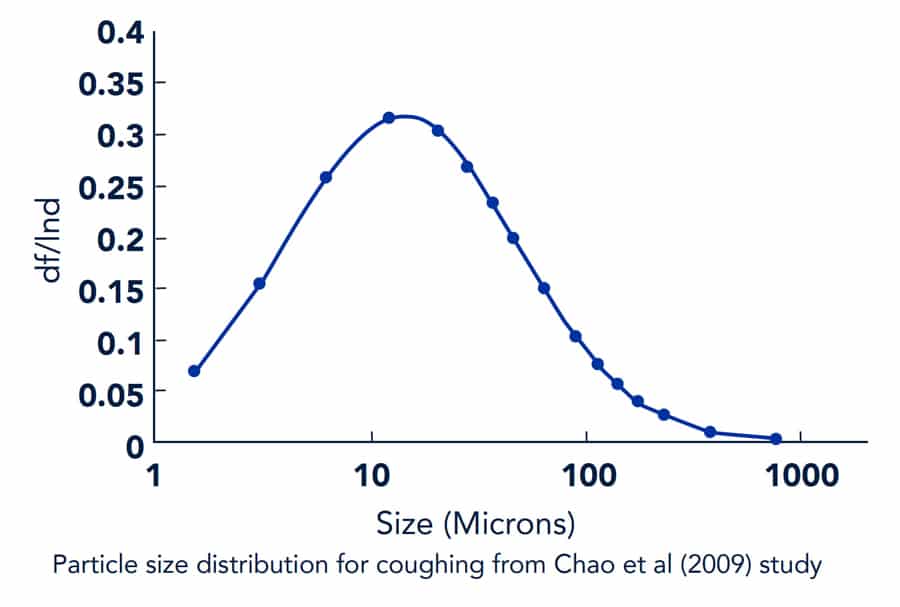
For coughing, this study used 16 different particle sizes and numbers as shown in the figure below (Chao et al, 2009). The total particle number per cough was 1,951. In addition, flow boundary conditions for breathing through the nose and coughing through the mouth were from Gupta et al (2011).
Study Results
The study findings show that elevator travel is a relatively low-risk activity. The high level of air exchange in an elevator lowers the risk of exposure, showing it to be comparable to a short time in an office or a bus. Mitigation strategies including masks and air purification using NPBI demonstrated a further reduction in risk.
Ventilation and Exposure
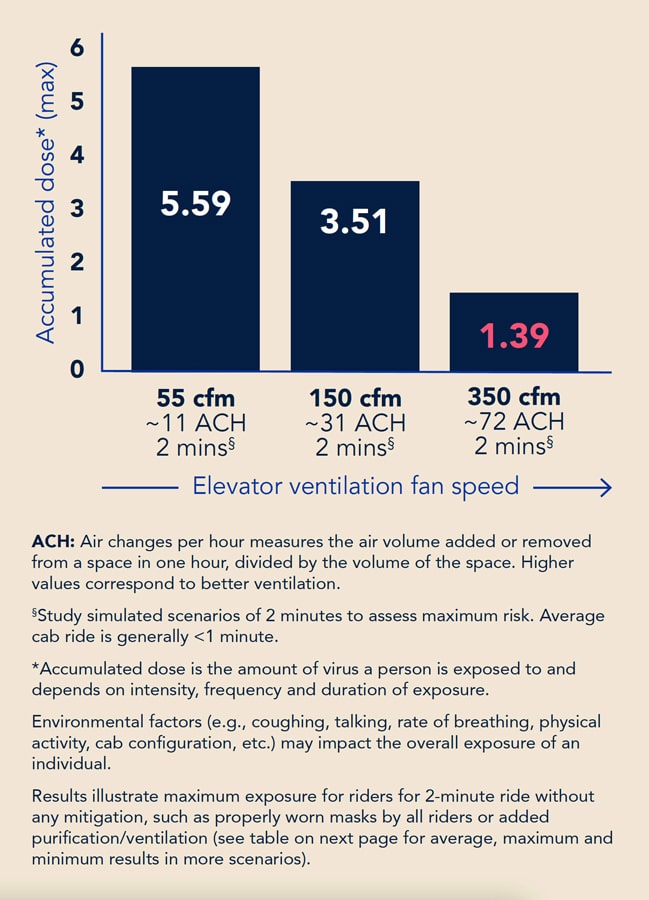
Due to the short duration of the elevator ride, elevators with high ventilation rates represented lower exposure risk. Although breathing generated particles continuously, the number and size of the particles were lower than those from a cough. The accumulated particle mass dose of the susceptible riders for the coughing case is up to six orders of magnitude higher than those for the breathing case.
The higher the ventilation rate, the lower the accumulated dose could be. However, this was not always the case, because, in a few cases, the nonuniform distributions of the particles could cause a higher dose, even with a higher ventilation rate. A deep cab could trap the particles inside the elevator. The air supply direction also had an impact on the particle dispersion in the elevator cab.
The exposure to the particles in the building lobby of floor 1 was low in this case, because the ventilation of the HVAC system and thermal plumes from the riders would cause the particles to disperse away from the riders and elevators. The movements of the riders could entrain some particles in their wakes. The particle distributions in the elevator cab were highly nonuniform. The person who stood in front of the index patient had the highest exposure, and the person who stood on the side of the index patient had the highest accumulated particle dose due to the longest exposure.
Comparisons With Other Activities
To better understand the true nature of the risk in an elevator, the study compared the quantitative results of accumulated dose in elevator scenarios with that in other common spaces and activities associated with office work. More specifically, we examined a bus with varying levels of air quality and an office environment. The focus is on the risk tied to airflow, with air exchange identified as a key factor.
The accumulated particle dose in a well-ventilated elevator with 350 ft3/min flow was equivalent to spending only 4 min in an office with 5 ACH of clean air. Even for an elevator with lower ventilation and 55 ft3/min flow, the dose for the ride was the same as 15 min in the office. The bus with 10 ACH outside air was relatively low risk, but the bus with 90% recirculated air posed more than 25 times the risk of the elevator.

When we take into account the duration of these activities, elevators become significantly lower risk by comparison. As noted, the average elevator ride lasts less than 2 min. An 8-h day in an office or 1 h on a bus was shown to yield exponentially higher accumulated doses.
The focus is on the risk tied to airflow, with air exchange identified as a key factor.
In addition to quantitative results, qualitative comparisons can give us a better sense of the relative exposure risk of riding in an elevator. The table below gives a general sense of where the relative risk of an elevator ride with and without mitigation may fall on a spectrum of other activities. It should be noted, however, that making quantitative comparisons to many different scenarios is difficult.

Even in controlled computer simulations, there can be a lot of variables, and both the natural and built environments have a lot of variation, especially when combined with human behavior.
The risk of dining at a restaurant, for example, varies based on number of diners, proximity, time spent in the space and other factors. Similarly, the risk associated with other indoor activities spans the spectrum due to variables related to both the environment itself and the behavior of occupants.
Still, with what we’ve learned, we can generally place riding an elevator in a relative low to medium risk of exposure: generally, a safe category comparable to a hotel room stay or outdoor dining, depending on the factors outlined.
Mitigation Strategies
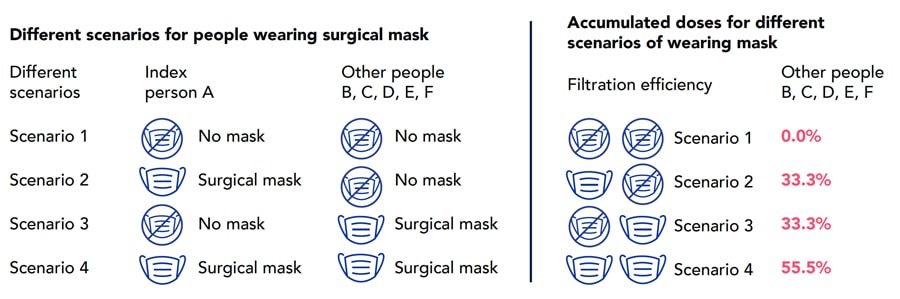
Although the study results show that elevators are among lower-risk indoor spaces for COVID-19 infection, any mitigation methods should be considered. This investigation considered two intervention methods: use of surgical masks and disinfection by NPBI.
This study selected surgical masks as an example to study the impact of masks on the accumulated dose of susceptible people. We assumed that the filtering efficiency for exhaled particles from the index patient was the same as that for inhaled particles by the susceptible riders. This investigation used a mean filtration efficiency of 33% for the surgical mask, according to Bowen (2010).
We can generally place riding an elevator in a relative low to medium risk of exposure; generally, a safe category comparable to a hotel room stay or outdoor dining, depending on the factors outlined.
Results indicated that if all the riders wore surgical masks, the dose can be reduced by 50%. This study assumed an index patient would cough once when entering the elevator. The cough would cause other riders inhaling approximately six orders of magnitude higher particle mass than continuous breath by the index patient for the duration of the ride.
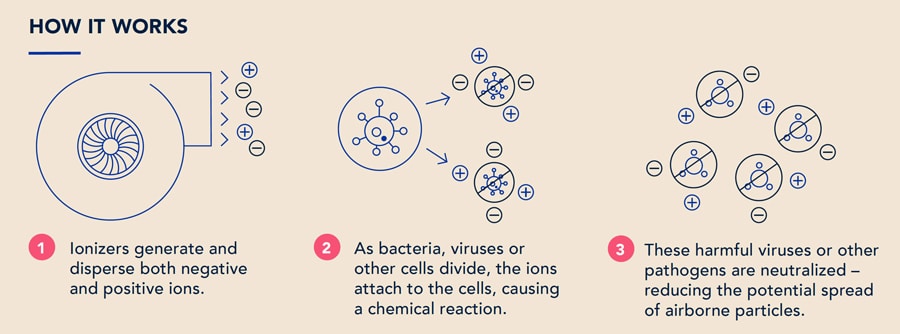
We also examined the impact of NPBI as a cab air purification method. Bipolar ionization is a technology used to improve air quality and lower the intensity of exposure that has years of research and test results supporting its safety and efficacy. Bipolar ionization emits both positively and negatively charged particles that attach to and deactivate harmful substances like bacteria, allergens, mold, viruses, volatile organic compounds and other particulates (Essien, 2017 and Hagbom, 2015).
In the case of bacteria and viruses, this chemical reaction both depletes their ability to function (by causing oxidative stresses within the organism) and causes physical destruction of their outer layer, effectively inactivating them. Particulate matter can be removed as air ions attach to them, causing them to become ionized and, in turn, attract other charged particles, increasing the rate of settling via gravity (Kim, 2017).
Our modeling indicated that the use of NPBI reduced risk to exposure 20-30%, depending on the ride time and riders’ positions within the elevator. Furthermore, the use of NPBI, combined with proper mask usage by all passengers, yielded a 60-65% reduction in relative risk.
Key Conclusions
This investigation used a combined CFD and multizone model to study airborne particle transmission of COVID-19 in taking an elevator in a typical office building with 35 floors. The CFD simulated the dispersion of the airborne particles exhaled by an index patient through breathing in the elevator ride. The multizone model was used to calculate airflow between floors and hoistway and airflow in and out of the elevator through cracks and small openings. The study calculated the accumulated dose of susceptible riders in taking elevators with the index patient under different conditions, such as different ventilation rate, air supply method, elevator cab geometry and intervention method.
Even in controlled computer simulations, there can be a lot of variables, and both the natural and built environment have a lot of variation, especially when combined with human behavior.
The intervention methods studied included wearing surgical masks by the riders and using NPBI technology in the elevator. This investigation also studied a case with a single cough from the index patient when the patient entered the elevator. For comparison, we also calculated accumulated dose for occupants staying 8 h in a typical office with 5 ACH clean air supply and a 1-h ride in a bus with 10 ACH clean air supply and 10 ACH air supply with 90% recirculated air. The study led to the following conclusions:
- Due to the short duration of the elevator ride, elevators with high ventilation had low risk. For the reference case with a 350 ft3/min ventilation rate, the highest accumulated particle dose by a susceptible person close to the index patient was 1.59.
- Because of the highly nonuniform distribution of the particles in the elevator cab, the accumulated dose was not inversely proportional with the ventilation rate. Dose was impacted by passenger position relative to the index patient. We also found a deep cab could trap a greater portion of the particles inside the elevator, and air supply direction had a negligible impact on the particle dispersion in the elevator cab.
- The dose in a well-ventilated elevator with 350-ft3/min flow was equivalent to a 4-min stay in the office with a 5-ACH clean air supply. Even for a poorly ventilated elevator with 55 ft3/min flow, the exposure for the trip was the same as a 15-min stay in the office. The bus with 10-ACH outside air was very clean, but the bus with 90% of circulated air was 25 times dirtier than the elevator air.
- Intervention methods can further reduce exposure. For example, by using bipolar ionization, exposure can be reduced further by 20-30% depending on the ride time and passenger position.
- The use of NPBI combined with proper mask usage by all passengers can further reduce exposure by 60-65%.
Limitations
This investigation had the following limitations:
- Since the numerical simulation of the entire process was very difficult, this study separated the whole process into eight sub-cases and transferred data after each sub-case simulation. Since the variables for each case could not be exactly the same, some errors may have been introduced.
- Since we need to simulate walking people, using a real-shaped person model would demand tremendous computing resources. In addition, Nielson (2003) found there was no big difference in heat transfer and flow between a real-shaped and simplified model. Therefore, this study used a rectangular column to simulate a person.
- We assumed the HVAC systems in the lobby of floor 1 supplied fresh air in the ceiling and that the lobby was connected with other spaces. Therefore, the outlets were assigned at the two connection walls. For the case we simulated, all the particles from the index patient moved upward and then to other spaces. The exposure of all other susceptible riders was almost zero. This may not always be true in reality as the waiting time of 30 s was relatively long. One should not neglect the impact of exposure on the susceptible riders.
- This study used a computer cluster to conduct the CFD simulations. Each simulation used two nodes with 24 processor cores per node on Intel Skylake CPUs @ 2.60 GHz. The memory per node was 96 GB. The average computing time for each sub-case was almost 12 h. That means each test case with eight sub-cases needed almost 100 h of computing time. The computational effort was significant.
Further Areas of Study
The project was a first phase of the elevator study initiated by Otis. After more than a three-month investigation by two full-time postdocs, this project has achieved the initial objectives. However, the research team and ad hoc review committee recommended the following areas for further study in the near future:
- Validation for the simulation results is essential. However, due to the short duration of this project, we conducted only numerical simulations for the particle distributions based on our previous experience. Experimental validation of the numerical results should be conducted.
- This investigation considered two intervention methods: NPBI disinfection and wearing masks. Other methods, such as photocatalytic oxidation, ultraviolet disinfection and HEPA filtering, should be examined.
- This study considered only the breathing and coughing scenario. However, the geometric diameter, size and number of particles generated by breathing, coughing, talking and sneezing are different. The mass of large particles due to talking, coughing and sneezing could be several orders of magnitude higher than that of breathing. It is important to improve the reference case design so the accumulated mass doses can be determined. It would be possible to determine a more definitive infection risk probability by working with epidemiologists and toxicologists.
- This project focused mainly on airborne particles, which the WHO, CDC and other experts have identified to be a more likely cause of infection risk. There are, however, other means of potential transmission we did not model in this study. For instance, since elevator spaces are very small, large droplets could be spread to the breathing zone via direct contact, or droplets could be projected due to momentum. This should be studied further.
- It is essential to consider the impact of different social distancing methods, especially the facing position of the riders with different loading capacity. The study has found the importance of the positions between normal and deep cabs.
- In addition, fomite contact should not be overlooked on elevators. Our simulations can determine particle deposition on different surfaces, such as elevator buttons and handrails. We should study if particle deposition would be a concern for infection transmission by fomite contacts.
- Our study has assumed the elevator cab would start in a clean condition. For frequently used elevators, the cab may already contain the COVID-19 virus. It would be beneficial to study if cabs should be disinfected before the next service and how long it takes to vent a cab to acceptable conditions.
- The current study used standard door closing/opening times. Air exchange when doors open, including the length of time doors are open, should be studied further. The study may include the impact of small pressure differences between the cab and landing area versus passenger drag. It could also examine whether it is better to make a straight shot to a destination (less time) or stop periodically and have more ventilation when there is an infected person on board.
Acknowledgments
Your authors would like to thank many named and unnamed collaborators who assisted with this work and continue to support ongoing efforts. Specifically, the research team expresses appreciation to those who helped review the work, including Dr. Richard Corsi and Dr. Elliott Gall of Portland State University, Dr. Darby Jack and Dr. Faye McNeill of Columbia University and Dr. Yuguo Li of the University of Hong Kong. Their critiques and recommendations have been visionary and will make the next phase of this study much better. We are also grateful to Rob Wheeler, Steve Kempf and Richard Pierce at Otis, who provided additional support.
References
[1] Allen, J.G. and Macomber J.D. “What Makes an Office Building ‘Healthy.’” Harvard Business Review (April 29, 2020).
[2] Allen, J.G. “Research: Stale Office Air Is Making You Less Productive,” Harvard Business Review (March 21, 2017).
[3] American Society of Heating, Refrigerating and Air-Conditioning Engineers. ASHRAE Handbook – HVAC Applications (SI), Atlanta, Georgia, USA (2007).
[4] American Society of Heating, Refrigerating and Air-Conditioning Engineers. Position Document on Filtration and Air Cleaning, reaffirmed by Technology Council on January 13, 2018, after initial publication on January 29, 2015.
[5] American Society of Mechanical Engineers. A17.1/CSA B44 Handbook on Safety Code for Elevators and Escalators.
[6] Axley, J. “Multizone Airflow Modeling in Buildings: History and Theory,” HVAC&R Research, 13:907-928 (2007).
[7] Bae, S.; Shin, H.; Koo, H.; Lee, S.; Yang, J. and Yon, D. “Asymptomatic Transmission of SARS-CoV-2 on Evacuation Flight.” Emerging Infectious Diseases, 26(11):2705-2708 (2020).
[8] Blocken, B. youtube.com/watch?v=MvLYHSODHVo (2020).
[9] Bolster, D.T., Linden, P.F. “Particle Transport in Low-Energy Ventilation Systems: Part 2: Transients and Experiments,” Indoor Air, 19:130-144 (2009).
[10] Buonanno, G.; Stabile, L.; and Morawska, L. “Estimation of Airborne Viral Emission: Quanta Emission Rate of SARS-CoV-2 for Infection Risk Assessment,” Environment International, 141 (2020).
[11] Centers for Disease Control and Prevention. cdc.gov/coronavirus/2019-ncov/faq.html#Spread (2019).
[12] Centers for Disease Control and Prevention DC/National Institute for Occupational Safety and Health. “Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation Guidelines for Healthcare Settings,” Publication No. 2009-105 (2009).
[13] Chao, C. Y. H., Wan, M. P. “A Study of the Dispersion of Expiratory Aerosols in Unidirectional Downward and Ceiling-Return Type Airflows Using a Multiphase Approach,” Indoor Air, 16:296-312 (2006).
[14] Chao, C. Y. H.; Wan, M. P.; Morawska, L.; Johnson, G. R.; Ristovski, Z. D.; Hargreaves, M.; Mengersen, K.; Corbett, S.; Li, Y.; Xie, X. and Katoshevski, D. “Characterization of Expiration Air Jets and Particle Size Distributions Immediately at the Mouth Opening,” Journal of Aerosol Science, 40(2):122-133 (2009).
[15] Chen, C.; Lin, C. H.; Jiang, Z. and Chen, Q. “Simplified Models for Exhaled Airflow From a Cough With the Mouth Covered.” Indoor Air, 24(6):580-591 (2014).
[16] Chen, C.; Zhao, B.; Cui, W.; Dong, L.; An, N. and Ouyang, X. “The Effectiveness of an Air Cleaner in Controlling Particle/Aerosol Particle Dispersion Emitted From a Patient’s Mouth in the Indoor Environment of Dental Clinics,” Journal of the Royal Society Interface, 7:1105-1118 (2010).
[17] Chen, C.; Zhao, B.; Yang, X. and Li, Y. “Role of Two-Way Airflow Owing to Temperature Difference in Severe Acute Respiratory Syndrome Outbreak in Hong Kong,” Journal of the Royal Society Interface, 8:699-710 (2011).
[18] Chen, J.; He, H.; Cheng, W.; Liu, Y.; Sun, Z.; Chai, C.; Kong, Q.; Sun, W.,; Zhang, J.; Guo, S.; Shi, X.; Wang, J.; Chen, E. and Chen, Z. “Potential Transmission of SARS-CoV-2 on a Flight From Singapore to Hangzhou, China: An Epidemiological Investigation,” Travel Medicine and Infectious Disease,
36:101816 (2020).
[19] Chen, Q. “Ventilation Performance Prediction for Buildings: A Method Overview and Recent Applications,” Building and Environment, 44:848-858 (2009).
[20] Chen, Q.; Zhao, S.L. and Liu, S. “Evaluation of COVID-19 Infection Risk When Taking Elevators,” Otis (December 2020).
[21] Cheng, V. C.; Wong, S.C.; Chuang, V.W.; So, S.Y.; Chen, J.H.; Sridhar, S.; To, K.K.; Chan, J.F.; Hung, I.F.; Ho, P.L. and Yuen, K.Y. “The Role of Community-Wide Wearing of Face Mask for Control of Coronavirus Disease 2019 (COVID-19) Epidemic Due To SARS-CoV-2,” Journal of Infection, (2020).
[22] Chin, A.W.H., Poon, L.L.M. “Stability of SARS-CoV-2 in Different Environmental Conditions,” The Lancet Microbe, 1(1):p. e10 (2020).
[23] Choi, E.M.; Chu, D.; Cheng, P.; Tsang, D.; Peiris, M.; Bausch, D.G.; Poon, L.L. and Watson-Jones, D. “In-Flight Transmission of SARS-CoV-2.” Emerging Infectious Diseases,” 26(11):2713-2716 (2020).
[24] Choudhury, D. “Introduction to the Renormalization Group Method and Turbulence Modeling,” Canonsburg, Fluent Inc. Technical Memorandum TM-107 (1993).
[25] Dai, H., Zhao, B. “Association of Infected Probability of COVID-19 With Ventilation Rates in Confined Spaces: A Wells-Riley Equation Based Investigation,” (2020).
[26] Darnell, M.E.; Subbarao, K.; Feinstone, S.M. and Taylor, D.R. “Inactivation of the Coronavirus That Induces Severe Acute Respiratory Syndrome SARS-CoV,” Journal of Virology, Methods 121, 85-91 (2004).
[27] Defile, N.C.; Allen, J.G.; Scheepers, P. and Levy, J. “The COVID-19 Pandemic: A Moment for Exposure Science,” Journal of Exposure Science & Environmental Epidemiology (April 29, 2020).
[28] Derwinski, T. “Safety Chain: A Look at Safety Systems in a Modern High-Rise Elevator in Light of 2018 Chicago Incident.” ELEVATOR WORLD (June 2019).
[29] FUJITEC Co. fujitec.com.ar/english/IHO_ionful.html (2008).
[30] GAMBIT CFD Preprocessor. User’s Guide, Lebanon, NH: Fluent Inc. (1998).
[31] Gao, N., Niu, J. “Modeling Particle Dispersion and Deposition in Indoor Environments,” Atmospheric Environment, 41:3862-3876 (2007).
[32] Gao, X.; Li, Y.; Xu, P. and Cowling, B.J. “Evaluation of Intervention Strategies in Schools Including Ventilation for Influenza Transmission Control,” Building Simulation, 5:29-37 (2012).
[33] Gupta, J.K.; Lin, C.H. and Chen, Q. “Characterizing Exhaled Airflow From Breathing and Talking,” Indoor Air, 20:31-39 (2010).
[34] Gupta, J.K.; Lin, C.H. and Chen, Q. “Transport of Expiratory Particles in an Aircraft Cabin,” Indoor Air, 21:3-11 (2011).
[35] Hang, J.; Li, Y. and Jin, R. “The Influence of Human Walking on the Flow and Airborne Transmission in a Six-Bed Isolation Room: Tracer Gas Simulation,” Building and Environment, 77:119-134 (2014).
[36] Hagbom, M.; Nordgren, J.; Nybom, R.; Hedlund, K.O.; Wigzell, H. and Svensson, L. “Ionizing Air Affects Influenza Virus Infectivity and Prevents Airborne-Transmission,” Scientific Reports, 5:11431 (2015).
[37] Hoehl, S.; Karaca, O.; Kohmer, N.; Westhaus, S.; Graf, J.; Goetsch, U. and Ciesek, S. “Assessment of SARS-CoV-2 Transmission on an International Flight and Among a Tourist Group,” Journal of the American Medical Association, JAMA Network Open, 3(8):e2018044 (2020).
[38] Hyun, J.; Lee, S.G. and Hwang, J. “Application of Corona Discharge-Generated Air Ions for Filtration of Aerosolized Virus and Inactivation of Filtered Virus,” Journal of Aerosol Science (2017).
[39] “iF World Design Guide.” ifworlddesignguide.com/entry/76697-mive.
[40] Jones, R.M.; Masago, Y.; Bartrand, T.; Nicas, M. and Rose, J.B. “Characterizing the Risk of Infection From Mycobacterium Tuberculosis in Commercial Passenger Aircraft Using Quantitative Microbial Risk Assessment,” Risk Analysis, 29:355-365 (2009).
[41] Khanh, N.C.; Thai, P.Q.; Quach, H.L.; Thi, N.A.H.; Dinh, P.C.; Duong, T.N.; Mai, L.T.Q.; Nghia, N.D.; Tu, T.A.; Quang, L.N.; Quang, T.D.; Nguyen, T.T.; Vogt, F. and Anh, D.D. “Transmission of SARS-CoV-2 During Long-Haul Flight,” Emerging Infectious Diseases, 26(11):2617-2624 (2020).
[42] Ko, G.; Thompson, K.M. and Nardell, E.A. “Estimation of Tuberculosis Risk on a Commercial Airliner,” Risk Analysis, 24:379-88 (2004).
[43] Kratzel, A.; Todt, D.; V’kovski, P.; Steiner, S.; Gultom, M.L.; Thao, T.T.N.; Ebert, N.; Holwerda, M.; Steinmann, J., Niemeyer, D., Dijkman, R., Kampf, G., Drosten, C., Steinmann, E; Thiel, V. and Pfaender, S. “Efficient Inactivation of SARS-CoV-2 by WHO-Recommended Hand Rub Formulations and Alcohols,” bioRxiv, (2020).
[44] Kujundzic, E.; Hernandez, M. and Miller, S.L. “Ultraviolet Germicidal Irradiation Inactivation of Airborne Fungal Spores and Bacteria in Upper-Room Air and HVAC In-Duct Configurations,” Journal of Environmental Engineering Science, 6:1-9 (2007).
[45] Launder, B.E., Spalding, D.B. “The Numerical Computation of Turbulent Flows,” Computer Methods in Applied Mechanics and Energy, 3:269-289 (1974).
[46] Li, X.; Niu, J. and Gao, N. “Spatial Distribution of Human Respiratory Particle Residuals and Exposure Risk for the Co-Occupant Under Different Ventilation Methods,” HVAC&R Research, 17:432-445 (2011).
[47] Li, X.; Niu, J. and Gao, N. “Co-Occupant’s Exposure of Expiratory Particles — Effects of Mouth Coverings,” HVAC&R Research, 18:575-587 (2013).
[48] Li, Y.; Qian, H.; Hang, J.; Chen, X.; Hong, L.; Liang, P.; Li, J.; Xiao, S.; Wei, J.; Liu, L. and Kang, M. “Evidence for Probable Aerosol Transmission of SARSCoV-2 in a Poorly Ventilated Restaurant,” medRxiv, 04.16.20067728 (2020).
[49] Liu, X., Wu, J., Liu, M., Dai, Y., Zhou, D., Li, W., Lv, P., Zhou, N., Wu, P. “Presymptomatic Transmission of COVID-19 in a Cluster of Cases Occurred in Confined Space: A Case Report.” 2020.
[50] Lim, T.; Cho, J. and Kim, B.S. “Predictions and Measurements of the Stack Effect on Indoor Airborne Virus Transmission in a High-Rise Hospital Building,” Building and Environment, 46:2413-2424 (2011).
[51] Lopez, G., Northrop, A. “How To Weigh the Risk of Going Out in the Coronavirus Pandemic, in One Chart,” Vox,
(vox.com/2020/5/22/21266756/coronavirus-pandemic-covid-risks-social-distancing-chart) (July 3, 2020)
[52] Mandavilli, A. “239 Experts With One Big Claim: The Coronavirus Is Airborne,” The New York Times (July 4, 2020).
[53] Marr, L., Corsi, R. “SARS-CoV-2 in Indoor Air: Principles and Scenarios,” Indoor air quality science and technology webinar presented by the U.S. Environmental Protection Agency, (epa.gov/indoor-air-quality-iaq/indoor-air-qualityscience-and-technology) (July 16, 2020)
[54] Mazumdar, S.; Poussou, S.; Lin, C. H.; Isukapalli, S.S.; Plesniak, M.W. and Chen, Q. “The Impact of Scaling and Body Movement on Contaminant Transport in Airliner Cabins,” Atmospheric Environment, 45(33):6019-6028 (2011).
[55] Mazumdar, S., Chen, Q. “A One-Dimensional Analytical Model for Airborne Contaminant Transport in Airliner Cabins,” Indoor Air, 19(1):3-13 (2009).
[56] Mazumdar, S.; Long, Z. and Chen, Q. “A Coupled CFD and Analytical Model to Simulate Airborne Contaminant Transmission in Cabins,” Indoor and Built Environment, 23:946-954 (2014).
[57] McDevitt, J.J.; Lai, K.M.; Rudnick, S.N.; Houseman, E.A.; First, M.W. and Milton, D.K. “Characterization of UVC Light Sensitivity of Vaccinia Virus,” Applied and Environmental Microbiology, 73:5760-5766 (2007).
[58] McDevitt, J.J.; Rudnick, S.N. and Radonovich, L.J. “Aerosol Susceptibility of Influenza Virus to UV-C Light,” Applied and Environmental Microbiology, 78:1666-1669 (2012).
[59] McLean, R. “The Mechanism of Spread of Asian Influenza: General Discussion,” The American Review of Respiratory Disease, 83:36-38 (1961).
[60] Megri, A. C., Haghighat, F. “Zonal Modeling for Simulating Indoor Environment of Buildings: Review, Recent Developments, and Applications,” HVAC&R Research, 13:887-905 (2007).
[61] Mitchell, B.W.; King, D.J. “Effect of Negative Air Ionization on Airborne Transmission of Newcastle Disease Virus[J],” Avian Diseases, 38(4):725-732 (1994).
[62] Morawska, L.; Tang, J.W.; Bahnfleth, W.; Bluyssen, P.M.; Boerstra, A.; Buonanno, G.; Cao, J.; Dancer, S.; Floto, A.; Franchimon, F.; Haworth, C.; Hogeling, J.; Isaxon, C.; Jimenez, J.L.; Kurnitski, J.; Li, Y.; Loomans, M.; Marks, J.; Marr, L.C.; Mazzarella, L.; Melikov, A.K.; Miller, S.; Milton, K.D.; Nazaroff, W.; Nielsen, P.V.; Noakes, C.; Peccia, J.; Querol, X., Sekhar, C.; Seppänen, O.; Tanabe, S-I; Tellier, R.; Tham K.; Wargocki, P.; Wierzbicka, A. and Yao, M. “How Can Airborne Transmission of COVID-19 Indoors Be Minimised?” Environment International, 142:105832 (2020).
[63] Murakami, S.; Kato, S.; Nagano, S. and Tanaka, S. “Diffusion Characteristics of Airborne Particles with Gravitational Settling in a Convection-Dominant Indoor Flow Field,” ASHRAE Transactions, 98(1):82-97 (1992).
[64] National Academies of Sciences, Engineering and Medicine. “Does Ultraviolet (UV) Light Kill the Coronavirus?” Based on Science, (nationalacademies.org/based-on-science/covid-19-does-ultraviolet-light-kill-the-coronavirus) (April 22, 2020)
[65] Nielsen, P. V. “Benchmark Test for a Computer Simulated Person,” Indoor Air 14.7. 2003:144-156.
[66] Noakes, C.J.; Khan, M.A.I. and Gilkeson, C.A. “Modeling Infection Risk and Energy Use of Upper-Room Ultraviolet Germicidal Irradiation Systems in Multi-Room Environments,” Science and Technology for the Built Environment, 21:99-111 (2015).
[67] Poussou, S.B; Mazumdar, S.; Plesniak, M.W.; Sojka, P.E. and Chen, Q. “Flow and Contaminant Transport in an Airliner Cabin Induced by a Moving Body: Model Experiments and CFD Prediction,” Atmospheric Environment, 44(24):2830-2839 (2010).
[68] Public Health Agency of Canada. “Prevention and Control for Health Care Settings: Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector.”
[69] Shao, S.; Zhou, D.; He, R., et al. “Risk Assessment of Airborne Transmission of COVID-19 by Asymptomatic Individuals Under Different Practical Settings,” Journal of Aerosol Science, 151:105661 (2021).
[70] Singh, N.; Kaczmarczyk, S. and Ehrl, T. “An Analysis of Airflow Effects in Lift Systems,” The 7th Symposium of Lift and Escalator Technologies, University of Northampton, U.K. (2017).
[71] Speake, H.; Phillips, A.; Chong, T.; Sikazwe, C.; Levy, A.; Lang, J., Scalley, B., Speers, D. J., Smith, D. W., Effler, P. and McEvoy, S.P. “Flight-Associated Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 Corroborated by Whole-Genome Sequencing,” Emerging Infectious Diseases, 26(12):2872-2880 (2020).
[72] Smagorinsky, J. “General Circulation Experiments with the Primitive Equations I: The Basic Experiment,” Monthly Weather Review, 91:99-164 (1963).
[73] Song, D.; Lim, H. “Application of the Mechanical Ventilation in Elevator Shaft Space to Mitigate Stack Effect Under Operation Stage in High-Rise Buildings,” Indoor and Built Environment, 23(1):81-91 (2014).
[74] Song, F.; Zhao, B.; Yang, X.; Jiang, Y.; Gopal, V.; Dobbs, G. and Sahm, M. “A New Approach on Zonal Modeling of Indoor Environment with Mechanical Ventilation,” Building and Environment, 43:278-286 (2008).
[75] U.S. Environmental Protection Agency. “Coronavirus Cases Trigger EPA Rapid Response” (epa.gov/pesticides/coronavirus-cases-trigger-epa-rapid-response) (January 29, 2020)
[76] Walker, C.M.; Ko, G. “Effect of Ultraviolet Germicidal Irradiation on Viral Aerosols,” Environmental Science & Technology, 41:5460-5465 (2007).
[77] Walkinshaw, D.S. “Germs, Flying and the Truth,” ASHRAE Journal, 52:70-73 (2010).
[78] Wang, J.; Chow, T.T. “Influence of Human Movement on the Transport of Airborne Infectious Particles in Hospital,” Journal of Building Performance Simulation, 8(4):205-215 (2015).
[79] Wang, L.; Dols, W.S. and Chen, Q. “Using CFD Capabilities of CONTAM 3.0 for Simulating Airflow and Contaminant Transport In and Around Buildings,” HVAC&R Research, 16(6):749-763 (2010).
[80] World Health Organization. Scientific Brief: “Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions,” (July 9, 2020).
[81] Xie, C.; Zhao, H.; Li, K.; Zhang, Z.; Lu, X.; Peng, H.; Wang, D.; Chen, J.; Zhang, X.; Wu, D.; Gu, Y.; Yuan, J.; Zhang, L. and Lu, J. “The Evidence of Indirect Transmission of SARS-CoV-2 Reported in Guangzhou, China,” BMC Public Health, 20(1):1-9, 2020.
[82] Xu, P.; Kujundzic, E.; Peccia, J.; Schafer, M.P.; Moss, G.; Hernandez, M. and Miller, S.L. “Impact of Environmental Factors on Efficacy of Upper-Room Air Ultraviolet Germicidal Irradiation for Inactivating Airborne Mycobacteria,” Environmental Science and Technology, 39(24):9656-9664, 2005.
[83] Xu, P.; Peccia, J.; Fabian, P.; Martyny, J.W.; Fennelly, K.P.; Hernandez, M. and Miller, S.L. “Efficacy of Ultraviolet Germicidal Irradiation of Upper-Room Air in Inactivating Airborne Bacterial Spores and Mycobacteria in Full-Scale Studies,” Atmospheric Environment, 37:405-419 (2003).
[84] Yakhot, V.; Orszag, S.A. “Renormalization Group Analysis of Turbulence,” Journal of Scientific Computing, 1:3-51 (1986).
[85] Young, L.; Wormser, G. “The Resurgence of Tuberculosis,” Scandinavian Journal of Infectious Diseases, Supplement, 93:9-19.
[86] You, R.; Lin, C.H.; Wei, D. and Chen, Q. “Evaluating the Commercial Airliner Cabin Environment with Different Air Distribution Systems,” Indoor Air, 29(5):840-853 (2019).
[87] Yu, L.; Peel, G.K.; Cheema, F.H.; Lawrence, W.S.; Bukreyeva, N.; Jinks, C.W.; Peel, J.E.; Peterson, J.W.; Paessler, S.; Hourani, M. and Ren, Z. “Catching and Killing of Airborne SARS-CoV-2 to Control Spread of COVID-19 by a Heated Air Disinfection System,” Materials Today Physics, 15:100249 (2020).
[88] Zhang, L.; Li, Y. “Dispersion of Coughed Particles in a Fully Occupied High-Speed Rail Cabin,” Building and Environment, 47:58-66 (2012).
[89] Zhang, R.; Li, Y.; Zhang, A.L.; Wang, Y. and Molina, M.J. “Identifying Airborne Transmission as the Dominant Route for the Spread of COVID-19,” Proceedings of the National Academy of Sciences (2020).
[90] Zhang, Z.; Zhai, Z.Q.; Zhang, W. and Chen, Q. “Evaluation of Various Turbulence Models in Predicting Airflow and Turbulence in Enclosed Environments by CFD: Part 2 – Comparison with Experimental Data from Literature,” HVAC&R Research, 13:871-886 (2007).
[91] Zhou, Y.; Shen, J. “Experimental and Numerical Study on the Transport of Droplet Aerosols Generated by Occupants in a Fever Clinic,” Building and Environment, 187 (2020).
[92] Zemouri, C.; Awad, S.F.; Volgenant, C.M.C.; Crielaard, W.; Laheij, A.M.G.A. and de Soet, J.J. “Modeling of the Transmission of Coronaviruses, Measles Virus, Influenza Virus, Mycobacterium Tuberculosis, and Legionella Pneumophila in Dental Clinics,” Journal of Dental Research, (9):002203452094028 (2020).
Stephen R. Nichols is a systems engineer with Otis at its Farmington, Connecticut, headquarters. Since March 2020, he has been the research, development and integration lead on the cross-functional global task force at Otis focused on pandemic response. This includes leading customer-facing rapid innovation, technology and product development, research, strategy and partnership efforts. Nichols is a two-time National Academy of Engineering Frontiers of Engineering alumnus and received the 2019 Gilbreth Lectureship. He has earned degrees in Mechanical Engineering from Tufts University and Rensselaer Polytechnic Institute and a professional certificate in Systems Engineering from Massachusetts Institute of Technology.
Dr. Sumei Liu is a postdoctoral researcher at Tianjin University in Tianjin, China. Her PhD thesis developed advanced models for accurate simulation of airflow in a building community. She received her BS from Hunan University in Hunan, China, and worked as a consulting engineer at Built Environment Group in Tianjin before pursuing her PhD at Tianjin University.
Dr. Xingwang Zhao received his BS from Chongqing University, China, and PhD from Tianjin University. He was a visiting scholar and postdoctoral researcher at Purdue University before joining Southeast University in Nanjing, China, for his second postdoctoral position. His past research included study and design of indoor thermal and air-quality environments using the adjoint method, which searches for boundary conditions according to the indoor environment design objective.
Dr. James T. Auxier leads global technology development at Otis, focused on emerging technology trends, business needs and strategic areas of technology development. He has experience in the building systems, aerospace and medical-device industries and university partnership and research experience, including 15 years focused on aerothermal technology development. He has earned degrees in Biomedical Engineering from Yale University, a master’s in Mechanical Engineering from Stanford University and a PhD in Biomedical Engineering from the University of Kentucky.
Tricia Derwinski has more than 30 years of experience in the development of systems, subsystems and components at Otis. Her areas of emphasis include the design, integration and development of cab shells and structural ceilings, and forced and natural ventilation. She was lead engineer for the modernization of the Empire State Building’s elevators, as well as the systems lead for numerous iconic buildings and major projects across the globe. She has a BS in Civil Engineering from Washington University and an MS in Mechanical Engineering from the University of Connecticut. She is a longtime member of both the National Elevator Industry, Inc. Performance Standards Committee and American Society of Mechanical Engineers (ASME) A17 International Standards Committee, as well as a participant in several International Organization for Standardization efforts related to lift and escalator ride quality.
Dr. Murilo Bonilha is director, system architecture, innovation and modeling, at Otis. Prior to joining Otis in December 2019, Bonilha worked at United Technologies Corp., where he led R&D programs on noise and vibration, software systems, power electronics and thermal and aerospace systems modeling. He was also general manager of UTC research centers in China and Ireland. He is a previous member of the Council on Tall Buildings and Urban Habitat China board and is a previous member of the Industrial Advisory Board of the USA-China Clean Energy Research Center. Bonilha has a Master’s in systems architecture and engineering from the University of Southern California and a PhD in acoustics and vibration from the University of Southampton in the U.K.
Dr. Qingyan (Yan) Chen is the James G. Dwyer professor of Mechanical Engineering at Purdue University in West Lafayette, Indiana, and the editor-in-chief of Building and Environment. Before he became the editor-in-chief of Building and Environment, he served as an associate editor of HVAC&R Research and was a member of the editorial boards of six other journals. Chen earned his Bachelor of Engineering degree in 1983 from Tsinghua University, China, and a Master of Engineering degree and PhD in 1988 from the Delft University of Technology (TU Delft) in the Netherlands. He conducted his postdoctoral research as a research scientist at the Swiss Federal Institute of Technology and worked as a project manager for TNO in the Netherlands. Before he joined Purdue University, he was a faculty member at TU Delft and the Massachusetts Institute of Technology (MIT). He has published three books and more than 470 journal and conference papers, and has been invited to deliver more than 170 lectures internationally.
Get more of Elevator World. Sign up for our free e-newsletter.